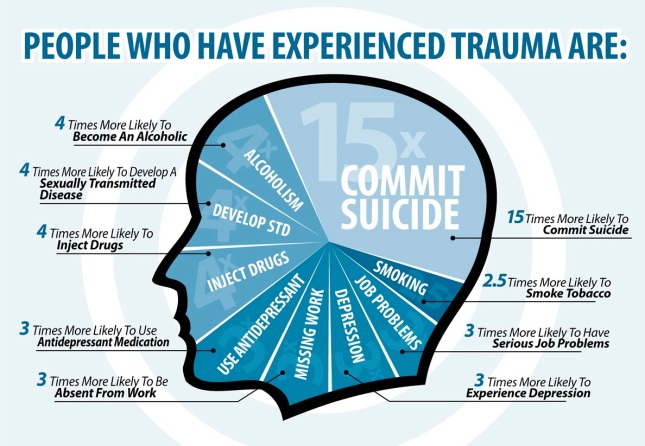
 I haven’t wanted to talk about trauma and how it impacts an individual; those who grieve in particular. I haven’t wanted to go there primarily because of the reaction one receives if they try to talk about it; skepticism. I’m not sure if people think they can simply look at a person and tell they are dealing with the after effects of trauma, or if they simply don’t believe it happens to people outside of the military and first responder communities. Who knows? The truth is we all experience trauma; usually in small, manageable degrees. Generally we ride it out, push through it, brush it off and move forward and beyond it. We remain standing and to the outside world appear largely unscathed. But sometimes we experience trauma of a far greater magnitude. Below are the sobering statistics of how people are affected by trauma:
I haven’t wanted to talk about trauma and how it impacts an individual; those who grieve in particular. I haven’t wanted to go there primarily because of the reaction one receives if they try to talk about it; skepticism. I’m not sure if people think they can simply look at a person and tell they are dealing with the after effects of trauma, or if they simply don’t believe it happens to people outside of the military and first responder communities. Who knows? The truth is we all experience trauma; usually in small, manageable degrees. Generally we ride it out, push through it, brush it off and move forward and beyond it. We remain standing and to the outside world appear largely unscathed. But sometimes we experience trauma of a far greater magnitude. Below are the sobering statistics of how people are affected by trauma:
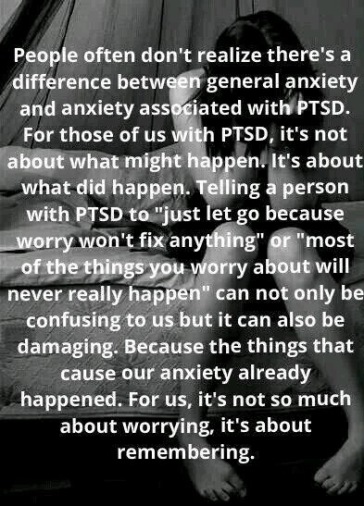
Traumatic experiences may or may not result in PTSD – Post Traumatic Stress Disorder. The general public understands little about this disorder. I understood little about PTSD and am slowly learning how it might impact an individual. What little people do know about the disorder has come from TV and movies and is usually, and justifiably so, attributed to military personnel who have seen and experienced frightful & life-threatening situations. Combat related PTSD generally results in the most severe effects and can dramatically alter an individual’s every day existence.
PTSD, like many other conditions, can be experienced in mild, moderate, severe or extreme forms. What most people don’t understand is that it can develop in an individual who lives in a continual state of heightened anxiety (soldiers on patrol who’ve never seen combat, individuals, especially children and family members who cope with life-threatening illnesses such as cancer, parents of special needs children, individuals who live in high crime neighborhoods or who have become refugees due to war or natural disasters all qualify) or PTSD can result from a single traumatic event.
If you asked a random group of people to describe the symptoms of PTSD, I imagine the single most common response would be the occurrence of flashbacks. A heightened sense of situational awareness is another common symptom of PTSD and I believe, the general public is vaguely aware that sounds, smells, and images can trigger disproportionate responses in those who suffer with PTSD. Less understood are the more subtle ways in which people who have experienced trauma internally process their experiences and the ways in which previous trauma changes an individual and therefore, how they cope with subsequent traumas.
Shock is an additional component closely related to trauma. One thing I didn’t understand about shock was the duration of time an individual might live and walk through life under the influence of shock. I didn’t understand that disassociation, a means of separating oneself from the events until one is capable of dealing with them, is what long-term shock looks like.
There was and continues to be a lot I don’t understand about shock and trauma. For one thing, people are amazingly resilient and for another, every individual is unique and can respond and react to the same trauma in unique ways.
So what kind of symptoms are commonly seen in individuals who suffer from PTSD?
*Extreme reactions (emotional and physical) to sights, smells or sounds (triggers) that remind the individual of traumatic events
*Avoiding people, places, and conversations related to the trauma
*Avoidance behavior designed to escape thoughts, memories and heightened levels of anxiety, abuse of alcohol, over-the-counter or prescription drugs, watching TV, spending time on the computer or reading excessively; anything that numbs pain or distracts the mind
*Experiencing feelings of emotional numbness or detachment, lack of interest in things previously enjoyed, guilt and blaming of self and others, depression
*Inability to concentrate, irritability and/or angry outbursts, difficulty sleeping
*Panic attacks involving intense fear, heart attack symptoms including chest pain, numbness, tingling, dizziness, shortness of breath, shaking, sweating and hot flashes
*Nightmares about an event
*Flashbacks (visions of a traumatic event where the individual feels as if they are reliving the experience while awake)
Aside from combat exposure, what kinds of trauma can precipitate PTSD? Surviving or witnessing situations involving extreme stress such as physical or sexual assault, natural disasters, torture, imprisonment, accidents and the sudden or unexpected loss of a loved one. Law enforcement officials, firefighters, paramedics, and medical professionals frequently deal with traumatic situations that make them vulnerable to PTSD.
There are several ways to lower the risk of developing PTSD. Support from family, friends, support groups and developing a coping strategy are chief among them. Surprisingly, how well an individual personally believes they responded during and immediately following a traumatic event or through the course of a series of lesser traumas plays a role in the development of PTSD. If an individual is able to act in a manner they perceive as effective during the traumatic event, if they feel good about their response in the face of danger, they are less likely to develop PTSD.
More than a year after the collision I received a CD from the McDonald County Dispatch Center of the 911 calls and the coordinated emergency response efforts related to the car wreck my family was involved in. It was disconcerting, to say the least, to hear my shrill voice in the background of two of the 911 calls reporting the accident. There was a definite tone of hysteria in my voice. However, the first emergency service provider who arrived on the scene, the Pineville Fire Chief, Gregg Sweeten, told me that when he approached me at the side of our minivan where I was kneeling and supporting Gracen’s head and shoulders, he thought I was a bystander who had stopped to help and had no idea that I was a passenger in the vehicle, let alone Gracen’s mother.
The grief counselor I see asked me how I felt about hearing that I was not initially identified as a victim. I hadn’t really thought about it from that perspective but I’m glad she asked because it led me to analyze my feelings. It helped me to realize that overall, I feel good about my response in the aftermath of the motor vehicle accident. There are things I wish I had the wherewithal to do, such as checking for a pulse or deciding if CPR should be started. But, I am thankful that I didn’t become hysterical to the point of inactivity or worse by far, to the place where my behavior prevented Gracen, David and O’rane from receiving needed medical care.
I’m glad I was able to help a bystander locate O’rane’s bag so the hospital would be aware of the medications he was taking. I’m glad I was coherent enough to explain to David’s mother the scope of our accident quickly over the phone. I’m glad I was able to tell the paramedics that Gracen is allergic to penicillin, to verbalize the medications she takes and the name and nature of her disease so the medical team might know about potential drug interactions, etc. Had I fallen to my knees screaming out my agony and despair emergency workers would have been distracted from caring for Gracen, and frankly, her life hung in the balance at that point in time.
I am beyond grateful that I was able to hold it together so that she got much needed medical attention and that I am not left with the suffocating knowledge and guilt that would have surely destroyed me had my reaction in the moments following the collision resulted in a failure for Gracen to receive prompt medical care resulting in her death.
I can’t say I’ve handled every traumatic experience in the way most beneficial to my daughter. There were moments when pain was not well managed well and I escaped Gracen’s hospital room, in effect abandoning her to the care of the medical staff and leaving David or my sister-in-law, Sandy, alone in the room to cope with this new trauma. How does a mother, or a father for that matter, determine if staying with their child when they are personally falling apart is more harmful to their child’s psyche than leaving the room so that the child doesn’t carry the burden of their parent’s despair along with their own? All I know for sure is that had another family member not been present, the staff would have had to drag me out before I would have left Gracen alone regardless of my state of mind.
Several years ago, I was driving home from dropping Gracen & Katie off at school when I heard a news report on the radio. The report stated that research had shown that long-term care givers were among those who suffered from PTSD due to the constant anxiety. I remembered thinking at the time, “I wonder if I have that?”
Looking back, and having become aware of lesser known symptoms of PTSD, I can see that not only was I actively practicing classic avoidance behaviors but that both Gracen and I were exhibiting emotional responses common to those who suffer from PTSD long before the collision that so impacted our lives. Observing the physical changes related to Gracen’s disease, coping with chronic daily migraines as well as complicated migraines coupled with painful medical tests, fears related to safety and an uncertain future took a toll. The most painful of which is the realization that the avoidance behaviors that allowed me to continue to perform day to day tasks while enduring the unrelenting anxiety also resulted in distancing myself from greater intimacy with my daughters.
Avoidance behaviors serve to insulate your heart from further pain and are a form of psychological protection. For example, consider the mother of a child who is undergoing cancer treatment. You may find her consistently present in her child’s hospital room. She brings a book or her tablet to occupy her time while her child sleeps or during times when her child is undergoing tests she can’t be present for, such as an MRI. As her child’s condition worsens you may notice that during times when her child is awake the mother may still be consistently present, may meet every physical need but personally engages less frequently. She may play with her smart phone while her child watches a movie instead of watching with them. She may read while her child colors a picture instead of coloring with them. She slowly and without conscious awareness, disengages from personal contact. The behavior that grants her a distraction from her worst fears and the lack of control also creates an emotional disconnect that is nothing short of emotionally devastating when she becomes aware of them.
This is the face of PTSD.
 Rarely can you identify an individual who is coping with PTSD by simply observing their behavior. Unless you are present when they encounter a trigger, have a flashback or wake up screaming in the middle of the night, PTSD can silently hide beneath a veneer of socially acceptable behavior.
Rarely can you identify an individual who is coping with PTSD by simply observing their behavior. Unless you are present when they encounter a trigger, have a flashback or wake up screaming in the middle of the night, PTSD can silently hide beneath a veneer of socially acceptable behavior.
Even when someone suffering from PTSD encounters a trigger or experiences a flashback you may not recognize the trembling hands, the internal panic, the flinch as gruesome images assault their minds. When they drop out of normal activities you may simply think they are grieving instead of recovering from a night without sleep or filled with nightmares. And how many people are privy to the methods of distraction utilized or the inability for those affected to perform simple tasks like returning phone calls, making appointments or paying bills?
Then shame takes center stage causing the individual to castigate themselves for all they can’t control or accomplish without understanding why the lesser known symptoms of PTSD are plaguing them. Unless they’ve seen a counselor they may not even know they have PTSD.
And of course, depression plays an active role as well. There’s also a difference between a mild or moderate case of depression and full-scale clinical depression. While the symptoms of mild and clinical depression are the same, the intensity of the feelings and the degree to which everyday life are impacted differ greatly. Common symptoms such as a change in sleep patterns (either sleeping too much or too little), new eating habits (evidenced by weight gain or weight loss), sadness, and a complete lack of motivation abound.
Outsiders look in and can’t understand why this person declines invitations. Why they don’t return to normal activities, get a job, or do any number of other things in order to help themselves never realizing the extreme melancholy, fatigue and shame often prevents them for taking the initiative to do anything. It takes too much energy or exposes their vulnerability to the outside world. Both are adequate deterrents by themselves.
Who wants to admit they are clinically depressed? Aren’t those people in institutions? Who wants to confess to struggling with PTSD? Isn’t that just a bid for attention? Who wants to admit that simple things are much too difficult – that they can’t quite cope – that they aren’t enough – that the awareness of their utter lack of control is terrifying?
Where is your faith, one might ask? Right where it always was, solidly grounded in my Savior, Jesus Christ. Then why can’t you trust in His loving care?
Consider Isaiah 43:2 with me.
“When thou passest through the waters, I will be with thee; and through the rivers, they shall not overflow thee: when thou walkest through the fire, thou shalt not be burned; neither shall the flame kindle upon thee.”
We like this verse because we concentrate on God’s promised care. But it seems to me that we only meditate on the “good” parts of the verse. We focus on the fact that the waters won’t overflow is, the fire won’t burn us or kindle a flame on us and that God will be with us, but we overlook or ignore the less desirable truth this verse reveals. We will be in deep water fighting to keep our heads above the surface. We will walk through the fire. And God will be with us – but we will still feel the water rise, we will still feel the heat of the flames. Experiencing PTSD and/or depression are not evidence of a failure to trust God, they are simply normal responses to trauma. PTSD, depression and anxiety, represent the deep waters and the firery flames of life’s tribulations. So we’d do well to recognize that it won’t be easy in spite of God’s presence. Additionally it will likely take a great deal of effort to try to respond in a Biblical way. Thankfully, there is love and grace and mercy when we stumble or outright fail to behave as we believe or expect we should.
There is hope of healing. Hope in making peace with an unknown future when experience has taught us that it will be painful. There is hope that we will exit the firery furnace without the stench of bitterness clinging to our hair and garments. There is hope that shock, depression, anxiety and PTSD will not define us but instead refine us, but oh, it’s a slow and painful process and we need to show ourselves grace along the way.
My personal prayer is that I will lower my self-imposed expectations. That I will be oblivious to the expectations and perceptions of others and that I will find overwhelming comfort in the unfailing presence and love of God, because the spirit is indeed willing but the flesh is oh so weak.
Melanie
December 4, 2015 at 1:49 am
So good! And so needful. Letting go of other’s expectations is hard- especially when we feel like we might be failing in our faith. Thank you for your honesty and courage to tell it like it is. I agree with you about the verse in Isaiah. Another one that I think we don’t fully embrace is from the Sermon on the Mount: not one sparrow falls without our Heavenly Father’s knowledge. But sparrows DO fall…
LikeLike
Peggy Duffy
December 15, 2015 at 12:14 am
Excellent article. I have struggled with this for 30 years.
LikeLike
James Rodriguez
July 2, 2019 at 1:58 pm
Thank you for this article. I do training on Trauma Informed Care and I wanted to know if I could use your graphic of the impact. Would you be able to tell me a little about? This looks like ACEs research. Is that correct. If so, can you tell me if you have more specific information about the number of ACEs associated with your numbers. Are all the probabiliites assoicated with 4 or more ACEs? 5 or More?
LikeLike
Janet Boxx
July 3, 2019 at 1:24 am
Mr. Rodriguez, thank you for stopping by and reading my blogpost. I’m encouraged to hear that training is being done on trauma informed care. What a positive difference such training can make in the care of patients who are suffering the effects of trauma!
In regards to the graphic, I can’t claim credit for it myself and I honestly had a difficult time determining who to attribute credit to. As best as I can determine the graphic originated with the Sandy Hook/Columbine Cooperative. I’ve included a link to their page below for your convenience. Hopefully, they can answer your questions regarding ACE research and the associated numbers.
Thank you for the work you do in educating others about the ways trauma affects individuals and providing care that is cognizant of and sensitive to those who have experienced trauma.
http://sandyhookcolumbine.org/behaviors-associated-with-traumatic-events/
LikeLike